Many people,– both female and male– experience issues with urinary incontinence which can be defined as unintentional leakage of urine. This can impact quality of life.
Urinary continence is the ability to control the bladder and prevent involuntary leakage of urine. This is an important aspect of daily life that affects physical, emotional and social well-being. Fortunately, physiotherapy can play an important role in managing or helping improve urinary incontinence through various techniques and exercises.
In 2024, it was estimated that 423 million individuals aged 20 and over worldwide experience urinary incontinence. So let’s learn a bit more about it and see where physiotherapy can help improve symptoms!
Myth: It is normal to pee a little bit when you sneeze, laugh or participate in exercise or movement.
Although it is very common, peeing when you sneeze, cough or exercise is not normal and you may have urinary incontinence. Urinary incontinence is the unintentional leakage of urine.

Myth: Only females that have given birth have incontinence.
Incontinence and leakage are widely believed to be a female issue, but males can also be affected. Studies conducted found that nearly 66% of men are unaware that they should complete pelvic floor muscle training. There is an under-reporting of symptoms within the male population and pelvic floor dysfunction due to stigma, embarrassment and the discomfort associated with discussing the issue.

Myth: My leakage will go away on its own.
With time, there is a chance that your leakage will get worse. Hopefully this article helps you understand what urinary incontinence is, and how pelvic physiotherapists can help improve your symptoms!
Here are the statistics:
- 1 in 3 females (child bearing and non-child bearing) have incontinence
- 1 in 9 males have incontinence, most commonly due to radical prostatectomies.
- Only 1:12 people will seek out treatment because they are embarrassed to talk about or don’t know the resources that are available.
What is the pelvic floor:
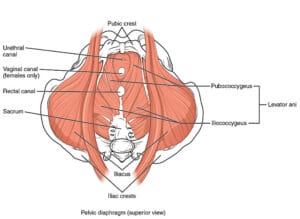
The pelvic floor muscles span from the bottom of the pelvis that support the core muscles, bladder and bowel for males and reproductive organs, core muscles, bladder and bowel for females. The muscles are like a hammock, tied to the front of your pelvis on one end, and your tailbone (coccyx) at the other. The pelvic floor muscles, act as a trampoline, moving up and down with breath. These muscles also work together to contract and relax when urination happens!
Functions of the Pelvic Floor:
- Bladder and bowel control
- Passing of urine and faeces
- Sexual function
- Pregnancy and Childbirth
- Pelvic organ support and Core muscle stabilization – Essentially, the pelvic floor is the floor of the core!
What is Urinary Incontinence:
Urinary incontinence is the involuntary leakage of urine which can sometimes happen due to pelvic floor muscle weakness or increased tension.
Risk factors for Urinary Incontinence include:
- Females
- Obesity
- Post-Menopause
- Pregnancy and Childbirth
- Having more than one child
- Obstetric trauma (from forceps, suction or tearing)
- Urinary or Gynaecological Surgery
- Chronic Illness
- Smoking
- Adolescent female athlete
- Males
- Radical Prostatectomy
- Prostate Enlargement
Types of Urinary Incontinence:
Stress incontinence: Involuntary leakage on effort or exertion (including sneezing or coughing). During exertion, your intra-abdominal pressure increases and your urethral sphincter in unable to keep the pressure being put on the bladder. This leads to leakage with everyday activities including lifting, laughing, jumping, sneezing or coughing!
Urge Incontinence: Also known as “overactive bladder” and is when you have a sudden urge to urinate, followed by involuntary leakage. An example of this could be when you come inside from a winter day, having the need to urinate when your bladder isn’t actually full.
Mixed incontinence: A combination of stress and urge, caused by an increase of pressure and the urge to urinate
Overflow Incontinence: The bladder doesn’t empty normally and becomes very full leading to constant dribbles of urine. The bladder may also never completely empty and is typically seen with conditions like Diabetes, Parkinson’s and after radiation to the pelvis.
Functional Incontinence: Urinary leakage caused by impairment of mental, cognitive or physical function) or environmental barriers that prevent timely access to the bathroom.
Post-prostatectomy Incontinence (PPI): Involuntary urine loss following prostate surgery.
What can a Pelvic Physiotherapist do for Urinary Incontinence?
- Create a safe and welcoming space for discussion: It is so important for clients to feel comfortable in the discussion of pelvic floor dysfunction and urinary incontinence as it may be embarrassing to talk about!
- Assessment/Education: Pelvic physiotherapists can conduct an internal pelvic exam to test the strength and functionality of your pelvic floor. They will also provide education on bladder habits, techniques from controlling incontinence and bladder irritants (yes, coffee is one!)
- Customize treatment plans: Just like our physical appearance, everyone’s condition is unique to them. Pelvic physiotherapist will provide individualized treatment plans, tailored to your goals and specific needs from the assessment.
- Biofeedback: In some cases, biofeedback or electrical stimulations may be used to assist with pelvic floor muscle training. This includes visual or auditory cueing to help client’s learn how to control and strengthen muscles. Electrical stimulation may also be used during a physiotherapy session to give gentle pulses to cue muscle contraction.
- Provide long-term solution: By addressing the causes of incontinence, pelvic floor physiotherapists will aim to provide long- lasting effects and improve quality of life.
- Help Improve confidence: Successfully managing incontinence through strategies provided by a pelvic physiotherapist may boost your self-worth, restore confidence and let you return to your daily activities without embarrassment or worry about leakage.
If you want to learn more about urinary incontinence, book an initial assessment with me today! Together we can come up with an individualized plan that works for YOU.
About the Author:

Shelby Cameron
Physiotherapist Resident
Book with Shelby at our Spadina Location!
References
Hirschhorn AD, Kolt GS and Brooks AJ. 2013. Barriers and enablers to the provision and receipt of preoperative pelvic floor muscle training for men having radical prostatectomy: a qualitative study. BMC Health Services Research. vol. 13, no. 1, pp. 305.
https://pelvichealthsolutions.ca/knowledge-base/incontinence-urinary-and-fecal
https://pelvichealthsolutions.ca/knowledge-base/facts-and-myths-about-pelvic-floor-dysfunction
https://www.jstage.jst.go.jp/article/jpts/26/9/26_jpts-2014-038/_pdf/-char/ja
https://www.ncbi.nlm.nih.gov/books/NBK559095/
https://www.physio-pedia.com/Pelvic_Floor_Muscle_Function_and_Strength

